'India Must Ensure Elders' Security, Sustenance, Access To Health'
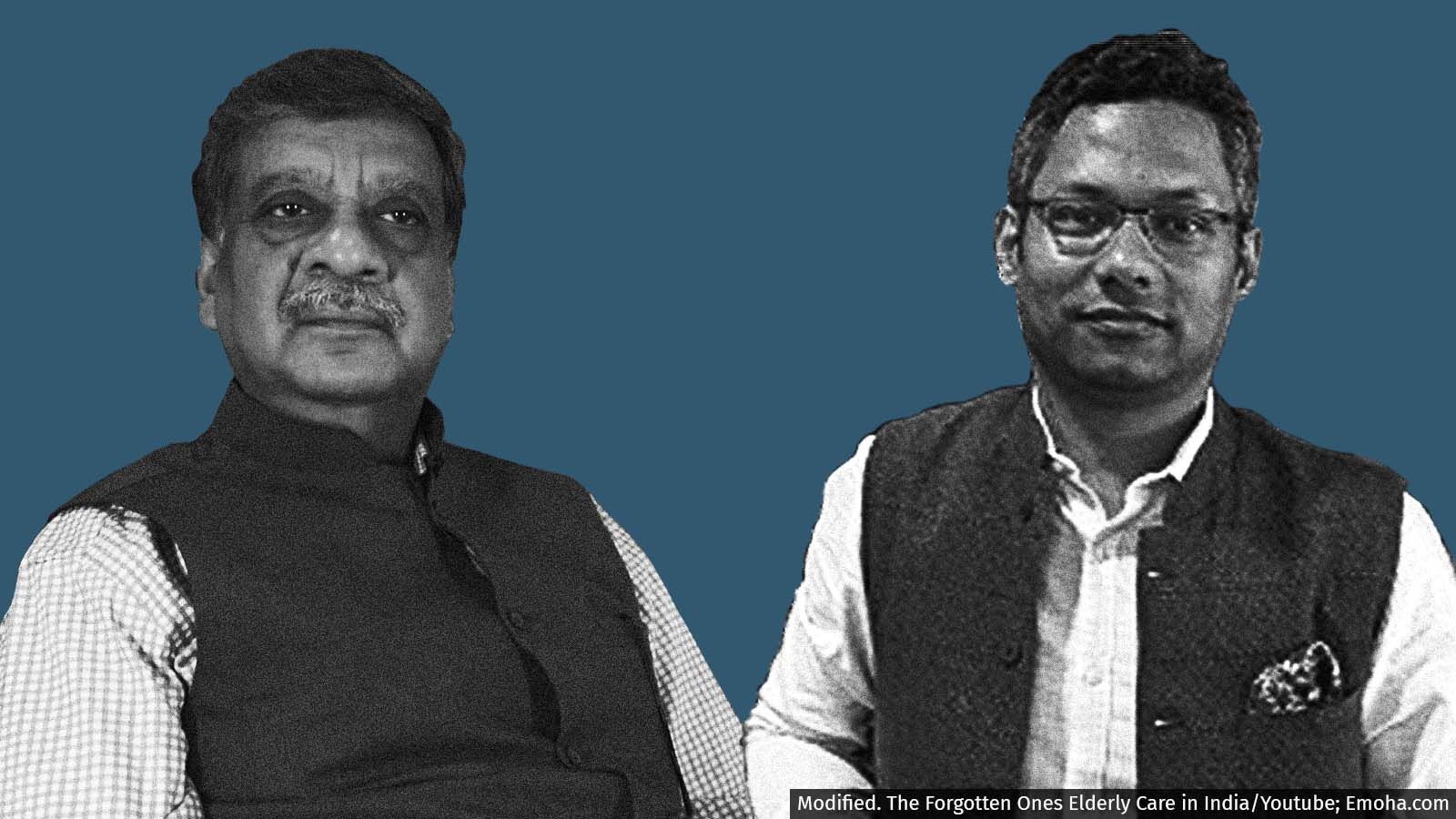
The pandemic has brought into the open the gaps in India's health policy, programme implementation, infrastructure and support systems for the elderly, who have been the most vulnerable to the virus. We spoke with A.B. Dey of AIIMS, Delhi, for the medical perspective and to Saumyajit Roy of Emoha ElderCare on the corporate response to addressing eldercare needs
Mumbai: India has the second largest population of elderly citizens in the world, currently estimated to be 137 million (of the 1.36 billion population). They constitute the fastest-growing segment of the population, expected to reach about 19% of the population in 2050. Yet, the health issues of India's elders have not been discussed as much over the last year and a half, in the post-Covid-19 era.
There is increasing anecdotal evidence about India's elders facing health issues, such as dementia and Alzheimer's, which were not witnessed as much in earlier decades. To discuss these concerns about eldercare, we spoke with A.B. Dey, professor of medicine and head, geriatric division, at the All India Institute of Medical Sciences (AIIMS), New Delhi, and Saumyajit Roy, co-founder and CEO of Emoha ElderCare, for the medical perspective as well as the corporate response to addressing eldercare needs.
Edited excerpts:
Dr Dey, tell us about India's healthcare response to elderly people aged over 60 years, particularly in light of the brutal second wave of Covid-19.
ABD: Older people suffered the maximum in the first Covid-19 wave, but in the second wave, the virus was not kind to any particular age group. It affected slightly younger people. The disease was severe among the 60-, 50-, 40- and 30-plus age groups. On how older people have been treated during the pandemic, let's understand that the disease started as a viral infection with a greater affinity towards older people in terms of rate of infection as well as outcomes like hospitalisation, need for intensive care, ventilator care and death. On all these parameters, older people fared very badly. Globally, 65% of deaths that occurred in the first wave--as well as a major part of the second wave--occurred in the 60-plus age group. In India, and in the South Asian context, the situation was similar.
Unfortunately, India's health system addressed the problems of older people with severe respiratory infections the way it treated younger people. When you compare outcomes for a 25-year-old and a 75-year-old put into intensive care or ventilator care, the chances of survival would be totally different. Because our experience with older people in acute care clinical settings is rather limited, India's health system response was also not correct in the initial phases. But I don't blame the system because we in the health system look at the whole population from a general point of view. This was so also when paediatrics was not separate. We were taught in medical school to cut a tablet in half and give it to a child. But then we understood that that's not that way, it's milligram per kilo of body weight and then the dosage is calculated. This was the reason why many of us did not opt for paediatrics, because remembering the dosage, etc. was a bit difficult. Similarly, most people consider older people as adults with a little bit of grey hair and wrinkled skin. But we understand much better now that it's a different ball game altogether, with dysfunctional organ systems and many other health issues which are steadily emerging.
One good thing that happened was that Covid-19 vaccination was targeted in the beginning--after the frontline workers--towards older people. This was the right step. Then the course correction [expanding vaccination to other age groups] was necessary as we have to vaccinate at least 85-90% of the population to reach that kind of immunity which will prevent further transmission. So with vaccination, older people had the advantage of getting vaccinated early, especially in India. Whereas that's not true for many neighbouring countries where older people were kept in the second or third position in the priority list while deciding the vaccination [cohorts].
About the Covid-19 pandemic vis-a-vis the older population, for the first time in India's health system, it was recognised that older people are a very vulnerable group in the face of such difficult diseases, pandemics and acute infection. The second thing that came up was that our health system, both public and corporate, is incapable of dealing with such acute diseases in such large numbers, especially among vulnerable and frail groups of citizens.
The only good thing that came out was that the scientific response to the infection in terms of devising a vaccine was very quick, and that the system saw to it that a large number of people have been vaccinated.
Mr Roy, you have been building an entrepreneurial response to eldercare. Tell us about the problems that you're trying to primarily address.
SR: I think 2020 and 2021 have truly opened the lid on the country's deepest secret--that our elders need to be taken care of. We always like to say that our elders are the foundation of our society. But as sons and daughters, as the 18 million NRIs across the world, saw the situation of their parents in different parts of India, the [gaps] in policy-making and ground implementation, infrastructure and support system came out in the open.
At Emoha, when we started the journey three years back, a year before Covid-19 hit the country, the whole idea was to look at how to take care of an elder in their own homes. Four trends emerged very clearly. One, the very important role of technology. It played a role during Covid-19, whether in the form of being able to access doctors from home via video conferencing, or making payments online. The 'connected community' concept is very strong. Therefore, the power of technology to deliver care in different parts of the country where elders might be alone is immense.
Second is the concept of 'ageing in place', which is the bedrock of what Emoha has been built on. This has gotten well established [during the pandemic]. Elders anyway want to stay at home, that's where they have their memories. Nobody wants to stay in a hospital. So ageing in place as a concept is about the ability to stream in resources required by the elders [into their homes], and not just during the Covid-19 stress test. If we can stream in a pizza, we can stream in other things as well.
Third is the role of the hyperlocal community, which I have seen become maximised in places where the government role got a little difficult. The local resident welfare associations, the chemist shops, the nurses and carers in the vicinity, those heroes came together. This really changed the potential [for ageing in place]. Through technology, all of this is very doable. This is exactly how we stitch [all these together] across 80 cities and towns, not just in Delhi. The community role becomes very powerful.
Last is the role of the corporates.
I see [what has happened] in a very positive way that while it is true that India has gone through a lot of difficulties [during the pandemic], it has shown some direction to both policymakers as well as sons and daughters abroad or in India, that if your parents have a protection system at home, if the technology is there, if the corporate is sensible and if the local community is stitched together, then there is hope. Then we have a chance of getting the elderly what they truly deserve.
Dr Dey, India has a National Programme for Health Care of the Elderly but one study IndiaSpend had reported on earlier showed that only 7% of the funds were actually utilised by the states and union territories. There seem to be many responses required, whether governmental or entrepreneurial or from hyper-local communities. Where do you feel India needs to focus its efforts?
ABD: From the healthcare point of view, I look at it this way. The National Programme for Health Care of the Elderly was started in 2010 with a lot of hope for the older population, as well as for the physicians working in this area, including me. But 10 years down the line, we found that the Indian way of addressing every crisis or every issue with a programme might not be working. As your report showed, hardly 7% of the budget could be spent. So there may be political will, programmes and budgeted funds, but utilising all the funds in the policy programmes for older people doesn't really happen.
I'll give you some statewise examples. In Karnataka or in Tamil Nadu, which have very good health systems, the programme performed very well. Even in a state like Rajasthan--not considered a very progressive state because it is clubbed in the BIMARU group--the programme had done very well with interventions. Maharashtra has shown this. I had once attended a meeting for the five districts in Odisha which were included in the first phase of the national programme. These were heavily Naxal areas in southern Odisha but the programme implementation was very good. But when you come to the North Indian states, the programmes don't work. So expecting a centrally created programme to trickle down to the last older person standing in the queue is not going to happen. Expecting that the funds that have been sanctioned and given to the National Health Mission (NHM), and the NHM will give it to the district and they will utilise it, that did not really happen and I don't expect it to happen either. If we create awareness in the health system that older people require some more intense or different kind of care, train our health professionals and provide that infrastructure, things will probably work out better.
Take the new programme of Health and Wellness centres under the Ayushman Bharat scheme, where one of the verticals is that of geriatric care for which I was initially involved in formulating the interventions. It has gone from a practical plan to a very idealistic programme of an ASHA worker with a 120-page manual visiting and addressing the problems of older people, along with all other programmes in all the 11 other verticals that she has to take care of. Probably this is not going to work though I pray that this family health and wellness clinic experiment succeeds.
Let's understand that the health services provided in the community, about 75% of outpatient care and 50% of inpatient care, come mostly from the private sector practising within the community. So, addressing only the public sector health system is not going to work, because either people do not have faith in it or it is not accessible. So the whole healthcare system, private as well as public, needs to be looked at. Also, [there needs to be] greater focus on human resources creation in the healthcare sector, starting from the undergraduate or qualifying training days; issues related to old age and vulnerabilities need to be incorporated into the curriculum.
Dr Dey, is there a changing profile of diseases the elderly are facing? I mentioned earlier increasing anecdotal evidence of elderly people facing dementia or Alzheimer's. Is it only that we're hearing of these now, or are these occurring more now? If so, what should be the policy and ground response?
ABD: I have lived and aged along with the ageing population. About three decades ago, when we started the service at AIIMS, seeing an 80-plus person was like seeing an animal in the zoo. How is it possible that this person survived all the childhood infections and poor access to the health system, etc., and lived till 80? Now, in our society, there are large numbers of people in their 80s and 90s. So as the population ageing has progressed, more and more older people are living to a very ripe old age, and rightly so. The diseases of that segment which were hitherto unknown to us are now unfolding. That's how we learn that this [disease] has [increased].
During my training in Newcastle in the UK in 1995-96, I used to consider that what people around me were talking about -- falls, syncope and dementia -- was all nonsense. I didn't see these. I only saw older people with high blood pressure, diabetes and infections. Then, when we started seeing people in their 80s and 90s, we found that these problems are very common, that older people have a propensity to fall and get fractures, and saw many such complications in the health system that started with a fracture and ended up on ventilators. Then we discovered that cognitive impairment or brain ageing is a major difficulty in caring as well as maintaining autonomy and independence for every individual. Nobody wants to be dependent on another human being for the basic functions of life.
In short, the diseases were there, the pathological process was always there. It's just that now that we have more people in the very old age group, we have started seeing them [more].
Mr Roy, how do you see eldercare evolving going forward and the ability of organisations like Emoha to respond and find solutions?
SR: I feel very optimistic about where we are. Twelve years back, when we had started the Association of Senior Living India industry body or the CII task force, which I was part of, the number of players in the eldercare industry, i.e. the silver economy sector, was very low. Today there are many players who have entered this segment and there is a lot of interest in this sector. I'll be very candid in saying that eldercare is not just healthcare. There is so much more to it.
As Dr Dey was saying, when you look at a 30- to 35-year span and do the math, how many days would you see a person being in a hospital or in a health [care-related] situation? About 85% of the time, they would be in a non-health [related] situation. Therefore, when you have a pillar of the economy with 30-50 years of experience, it can give a boost to the country's talent pool. We have a large population of millennials who can benefit from the kind of experience that elders can bring to the table, whether it is counseling or developing emotional skills -- all the kinds of softer abilities which sometimes our younger population lack. So, I see a lot of opportunities for different segments within the silver economy, which cannot be painted as only healthcare.
Even at Emoha, healthcare is a large part of what we do. We take care of emergencies, we've saved 170 lives, we have a lot of doctors and specialised care. But we also take care of emotional wellbeing. We also have different types of solutions towards engagement, activities, events, and so on.
So the startups in the eldercare space are starting to show opportunities which can become potentially unicorns as we go forward, because this is a segment of the population that is close to about 110 million today, going to become 340 million, whose consumption is anywhere between Rs 15,000-20,000 to Rs 1 lakh per month. So, this is a Rs 40,000-50,000 crore [$5.4-6.8 billion] market opportunity. Done well, with the right kind of player with the right intent, there are micro niches from infrastructure creation, to artificial intelligence- and machine learning-oriented [opportunities], from data sensors in the home to healthcare at home. All these segments will see growth as we move forward, and they will complement the efforts of the government. [There could] potentially be even public-private partnerships. In different parts of the country, different [government] initiatives can get support from the private sector as well. So I'm quite bullish. I think Emoha has seen a lot of growth in the last two years and I see the next couple of years being the fruition of whatever we have seen in edu-tech or health-tech translating into the age-tech field.
Dr Dey, as you said, what are policy efforts that India should do, from a policy point of view, to address this going forward? And on a micro level, what would your message to young people be on how they could look after their ageing parents better?
ABD: In terms of the policy component, what we need for a person to age and live happily is some minimum resources for sustenance, access to a fairly competent health system, and security in the society, including in the family.
I've seen national policy since 1999. A lot of things have happened, and let's understand we are a big population so obviously, I don't expect that every senior citizen in the country will be provided for. But there is a positive inclination in the minds of policymakers and programme managers now. As I have interacted with these people for decades, now I see that those who are in their late fifties are understanding that they're doing this for themselves.
On the societal challenges that ageing populations bring and how we address them, this started as a World Health Organization proposal and has now become a United Nations' proposal: the UN Decade of Healthy Ageing from 2021 to 2030, coinciding with the Sustainable Development Goals endpoint of 2030.
As Saumyajit said, just look at innovation and unleash the energy and wisdom of older people. That will provide great resources to society. We need to think in a different manner than what we are used to, the usual World Bank thinking that this is a kind of wasted investment. It's not, because as a caring society, you cannot have 10% of your population in deep misery and the rest 90% living happily. That doesn't happen.
For the younger generation, do consider that you will be older people in the next three decades. So take care of your own health, sustenance and survival when you are 60 plus, and also look at those who have already reached there and support them with the three things that I named--sustenance, security and access--so that they are also happy. All younger people should plan, from now, how to remain healthy in their 60s, 70s and 80s, so that their need for hospital care and for support is minimised. The last line that the UN decade pledge says, leave no one behind, that's important. We must look collectively at the whole population of older people as well as the younger generation who are going to reach that segment, and leave no one behind.
We welcome feedback. Please write to respond@indiaspend.org. We reserve the right to edit responses for language and grammar.


