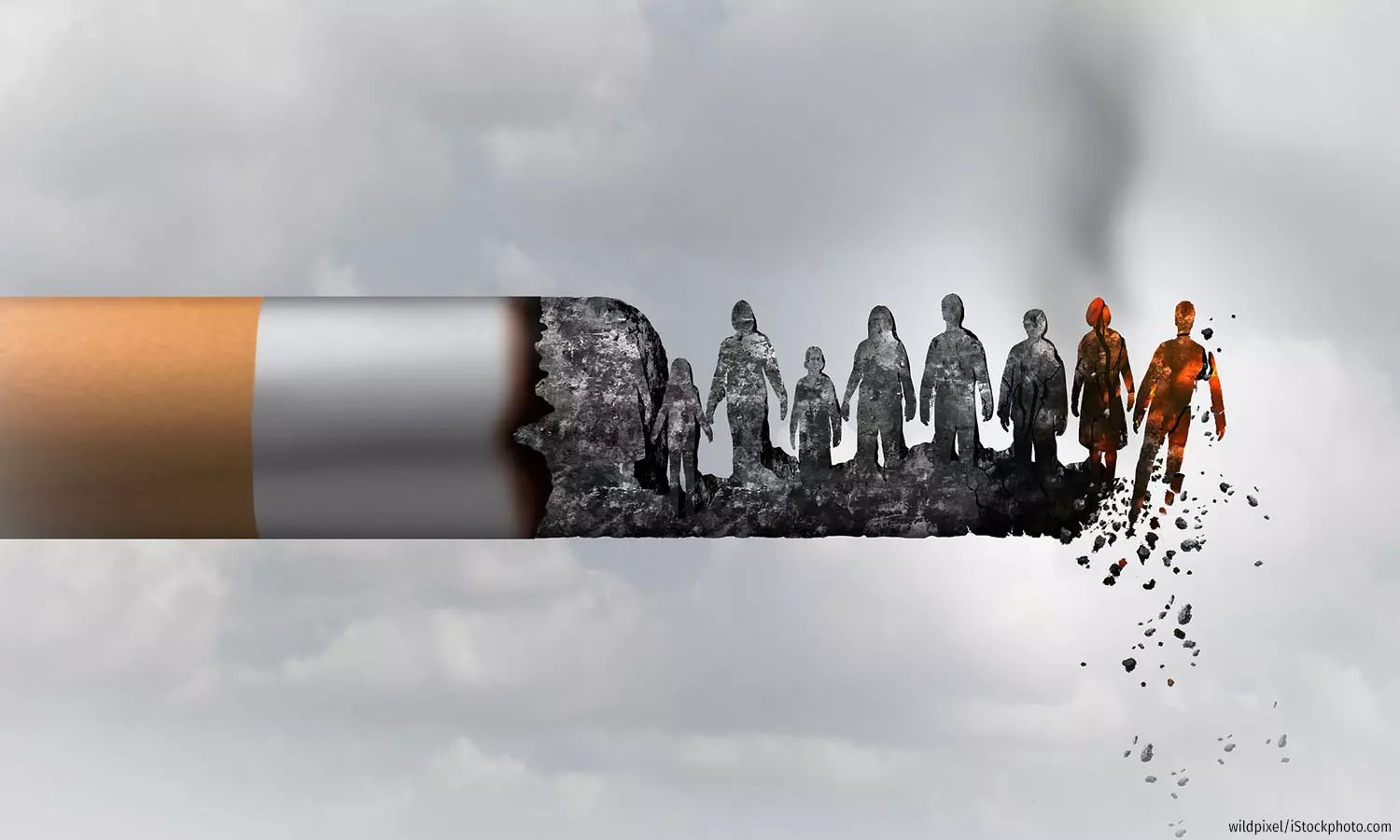
In 2020, 225,000 Indians Died Of Cancer From Preventable Risk Factors
Tobacco smoking and HPV infections caused the highest number of preventable cancer deaths
Mumbai: In 2020, more than 225,000 Indians died of cancer caused by preventable risk factors, a recent study has revealed. The study, which analysed data from Brazil, Russia, India, China, South Africa, the United Kingdom, and the United States, found that India had the second highest number of such cancer deaths, following China, which had 1.1 million deaths.
Published in the Lancet in November 2023, the study was conducted by researchers from universities and research centres in six countries, including the Indian Council of Medical Research (ICMR), the International Agency for Research on Cancer (IARC), Queen Mary University of London, and King's College London. They studied cancer deaths due to four major preventable risk factors: tobacco smoking, human papillomavirus (HPV) infection, alcohol consumption, and excess body weight. These seven countries represent more than half the burden of cancer deaths across the globe.
The study also compared the years of life lost (YLLs) due to cancer caused by these preventable causes. YLL is an estimate of the average years a person would have lived if they had not died prematurely. It helps quantify the societal impact of premature deaths from diseases. The research concluded that India lost around 4.2 million YLLs due to cancer caused by avoidable reasons, only behind China, which lost 18.5 million YLLs in 2020.
However, when standardised for age structures across countries, India had the lowest mortality rate (32.3 deaths per 100,000 population) and YLL rate (582.6 years lost per 100,000 population). China had the highest (93.4 deaths and 1,560.9 years lost per 100,000 population).
Globally, men had higher age-standardised YLL rates for cancers due to tobacco smoking and alcohol consumption, while women had higher rates for cancers from HPV infections and excess body weight. In India, men’s age-standardised YLL rates from tobacco smoking and alcohol consumption were nine and seven times, respectively, the rates among women. For cancers from excess body weight and HPV infections, women had six times and 12 times the rates as men.
India’s cancer burden is expected to rise to 2.09 million new cases in 2040 from 1.32 million in 2020, according to IARC estimates. Similarly, the deaths caused due to cancer are also projected to rise to 1.38 million in 2040 from 852,000 in 2020.
In an award-winning series in 2017, IndiaSpend examined the country’s cancer care crisis. We had surveyed 51 patients living on the pavement outside Mumbai's Tata Memorial Hospital, to try and quantify the stress on financially vulnerable households. On average, the patients surveyed had not worked for a year and lost Rs 55,000 in income. One in four borrowed from relatives and moneylenders, and spent Rs 76,000, on average, before ending up on the pavement. Further, 92% had a grade VII education or less.
India has one oncologist for 1,500 patients (in the US, it is one per 100 and in the UK one per 400), and they are concentrated in about eight metropolitan cities, according to a 2015 study by the consulting firm Ernst and Young, we reported. Mortality rates are higher than the West because of late diagnosis and treatment and the prevalence of cancer is likely to rise as Indians age, become more obese, smoke, drink more liquor, breathe polluted air and drink polluted water.
IndiaSpend reached out to the Ministry of Health and Family Welfare for comment on the study’s findings. We will update this story when we receive a response.
Tobacco smoking, alcohol consumption leading cause of cancer deaths
Tobacco smoking and alcohol consumption emerged as the largest contributors to preventable cancer deaths and YLLs in all seven countries, the study found.
Of the 30 million YLLs from cancer due to these risk factors, tobacco smoking contributed to 20.8 million and alcohol consumption to 5.9 million. In India, tobacco smoking led to more than 110,000 cancer deaths--nearly half the deaths from all four factors--and 1.8 million YLLs in 2020. Alcohol consumption contributed to over 41,000 deaths and 835,000 YLLs.
Across the seven countries, tobacco smoking was mostly associated with lung cancer, while in India, most YLLs due to tobacco smoking were from head and neck cancers in men and gynaecological cancers in women.
“We see the largest amount of head and neck cancer all over the world, and ours is, most of the time, tobacco-related problems,” said Boman Dhabhar, Director of Medical Oncology at Mumbai’s Fortis Hospital. “I totally agree there is a human papillomavirus component even in head and neck cancer, but it is mostly related to tobacco products.”
How does tobacco use cause cancer?
“It is crucial to grasp that cancer is nothing but an abnormal cell. It's been part of your body initially; it has become abnormal, and it has started growing,” explained Uma Dangi, medical oncology consultant at Mumbai’s Fortis and Hiranandani hospitals. “It becomes abnormal because it acquires certain mutations in its genes or in its DNA to replicate rapidly without the control of the body, which usually controls it. So it becomes autonomous, sort of, and it grows on its own uncontrollably.” Tobacco, in its various forms, contains many harmful chemicals that make the normal body cells prone to such mutations, increasing the risk of cancer, Dangi explained.
Among Indians aged between 15 and 49 years, approximately 39% men and 4% women use some form of tobacco, according to National Family Health Survey 5 (NFHS-5) data, declining from 45% and 7%, respectively, in 2015-16. Rural India saw a higher prevalence of tobacco use.
The study only looked at mortality from tobacco smoking. In India, chewing is the principal form of tobacco use, said Monika Arora, Vice President (Research and Health Promotion) at the Public Health Foundation of India (PHFI). About 186 million Indians chew tobacco, comprising 68% of the global number, a 2021 study found. Overall, tobacco-related cancers accounted for 27% of India’s 1.39 million cancer cases in 2020, data from the National Cancer Registry Programme show.
In contrast, only about 1% of women and 23% of men aged 15-49 years currently drink alcohol in India, according to NFHS-5. Among women who drink alcohol, 17% drink alcohol almost every day and 37% drink alcohol about once a week. Among men who drink alcohol, 15% drink alcohol almost every day, 43% drink alcohol about once a week, and 42% drink less often than that.
Alcohol has many harmful effects on the human body. It can lead to cardiac arrests, other heart-related ailments, and liver issues, specifically liver cirrhosis, which can prove to be fatal. Thus, alcohol has a compounding effect, making it difficult to pinpoint that any death is an alcohol-related cancer death, explained Dhabhar.
Again, head and neck cancers contributed to the most alcohol-related YLLs among Indian men, while oesophageal cancer was most common among women.
HPV infections led to 89,000 cancer deaths
HPV emerged as the second largest preventable cause of cancer deaths in India, according to the study. It led to 89,000 deaths and 1.7 million YLLs in 2020.
HPV is a group of more than 200 related viruses. Some of these viruses have been linked to 15 types of cancer. Although it is a commonly found virus and is usually cleared by the body, sometimes it gets to the cells of the affected area, gets into its DNA and leads to changes that might cause precancerous lesions or cancer, explained Dangi.
Women had a higher prevalence of HPV-related cancers compared to men. For India, the age-standardised YLL rate for women was 12 times higher than for men. HPV-related cancers led to 82% of female YLLs from all four factors in the country.
Cervical cancer contributed to the most YLLs from HPV infections among women in all seven countries, while head and neck cancers were most common among men.
Cervical cancer is the second most common female cancer in India--after breast cancer--accounting for 10% of all female cancers, IndiaSpend reported in December 2023. Regular screenings allow cancer to be detected earlier, sometimes in a precancerous stage when it can be treated easily, said Dangi.
Excess body weight growing cause for concern
India recorded around 8,000 cancer deaths due to excess body weight in 2020, accounting for 3.5% of cancer deaths from preventable reasons. This was the lowest number after South Africa, which saw 3,800 such deaths.
“Overweight and obesity are increasing at a rapid pace in India. So if you look at underweight and malnutrition, the rate at which those numbers are declining, the overweight and obesity are increasing more rapidly,” said Arora from PHFI.
In India, among adult men and women, the prevalence of underweight saw large reductions between 2005-06 and 2015-16, but a doubling in overweight and obesity was also recorded over the same period. In 2019-21, 23% men and 24% women aged 15 to 49 years were overweight or obese, NFHS-5 shows. Owing to these trends, India might record an increased burden of cancer due to excess body weight in the coming years, Arora added.
Across all seven countries, colorectal and other gastrointestinal cancers contributed to the most YLLs from excess body weight among men, while breast cancer was most common among women.
Policy changes can help reduce cancer deaths, expert say
In response to the global problem of cancer deaths caused by tobacco consumption, the World Health Organization (WHO) launched the Framework Convention on Tobacco Control, which recommends legal guidelines for countries to follow regarding tobacco taxation, smoke exposure protection, product packaging and labelling, and advertising/sponsorships. India is also a signatory to the framework, but its taxation is below the recommended levels.
Despite the 28% goods and services tax levied on tobacco products, the effective tax as a percentage of retail price falls significantly short of the WHO's recommended level of 75%. Specifically, cigarettes are taxed at 53%, bidis at 22%, and smokeless tobacco at 60%--all falling well below the recommended threshold.
“Taxation definitely has a lot of scope in India to make the products expensive so that they are unaffordable for experimentation among adolescents and also to protect the poor from the dangers of tobacco use,” Arora said.
Further, India scored 58, and ranked 40 of 90 countries, in the 2023 Global Tobacco Industry Interference Index. Article 5.3 of the WHO Framework Convention on Tobacco Control states that there should be no incentive given to the tobacco industry. India had “ample instances of unnecessary interaction of top-level government officials with tobacco companies and front groups”, the report found.
In July 2020, the Union government released a five-page code of conduct for government officials to prevent tobacco industry interference in public health policies. But the code comes with a built-in limitation: it is only applicable to health ministry officials despite the fact that the influence of the tobacco industry in public policy is far more widespread, IndiaSpend reported in December 2020.
Cancer caused by excess weight is already a problem in countries like the USA and UK. In India, obesity and overweight cases are increasing at an alarming rate, and it may become a concern in the coming years. India is already tackling the undernutrition problem in the country, making it a multi-faceted issue.
“Our programming needs to be more balanced, which means we are addressing undernutrition in various programmes. It is time we start looking at both obesity and undernutrition,” explained Arora. “This is called looking at syndemic solutions. So, a syndemic is when you look at overweight, obesity and undernutrition in the same country and give programmes and interventions that address both ends of the spectrum.”
In the case of cancers caused by HPV, the most effective ways to contain cancers are early detection via screenings and vaccinations, both of which have remained low across the country. Due to a lack of awareness and trained personnel, screening remains low across the country, said Dangi.
In 2020, the World Health Organization (WHO) set a 90-70-90 Cervical Cancer Elimination Strategy Target for 2030, our December 2023 report noted. Essentially, the target mandates vaccinating 90% of girls with the HPV vaccine by the age of 15, screening 70% of women with a high-performance cervical cancer test by 35 years of age and again by 45 years of age, and treating 90% of women identified with cervical disease. HPV is associated with pre-cancerous lesions that may become cervical cancer but a preventative vaccine exists.
Less than 2% of women aged 30-49 years have ever been tested for cervical cancer, according to NFHS-5. Low awareness and the social stigma associated with the disease adversely impact the uptake of screening and treatment, and a delayed vaccine roll-out is costing lives, we reported.
“I think that there is a sort of a lack of awareness among people, so they don't come forth with the screening, they don't come forth even when they have symptoms,” Dangi said. The first step would be to create large campaigns for awareness amongst the community that it is important to get yourself screened. It should be sort of a mandatory health check.”
A 2020 survey by Cancer Awareness, Prevention and Early Detection Trust revealed a lack of awareness and action regarding cervical cancer. Among 1,305 participants, only 45% were aware of the term ‘cervical cancer’, and 34% were correctly aware that it occurs in the uterus.
Two HPV vaccines are available in the Indian market, but price and accessibility are roadblocks. In December 2022, the National Technical Advisory Group for Immunization recommended the introduction of the HPV vaccine in the Universal Immunization Programme (UIP), we reported in December 2023. Globally, about 96 countries have included the HPV vaccine in their immunization programmes. Now, authorities said that the inclusion of the HPV vaccine in the UIP has been sanctioned but they are working on the modalities.
“We’ll start the rollout when we have enough vaccine available, when we are ready for it,” Veena Dhawan, Additional Commissioner (Immunization), Ministry of Health & Family Welfare had told IndiaSpend.
We welcome feedback. Please write to respond@indiaspend.org. We reserve the right to edit responses for language and grammar.


