Your Poisoned Food, Our Unending Greed

Akhilanand Mishra will never forget how he found his son Ashish Kumar, “vomiting and with diarrhoea”, indications that the five-year-old child’s body was trying to expel poisons after eating his government-provided midday meal in July 2013.
“I rushed my son to the government hospital, where there was no bed, then to a private hospital, where too there was no bed,” Mishra, 42, a shop-keeper, told IndiaSpend in an interview. “By then the authorities had woken up to the tragedy, and we were advised to take my son to the government hospital. He died en route.”
Ashish was one of 23 young lives lost in Bihar’s Dahrmasati Gandawan village to the carelessness of headmistress Meena Devi. They died after eating contaminated food—the midday meal meant to nourish them.
Meena Devi had stored raw ingredients for the meal next to toxic pesticides and organic manure and the cooking oil in an empty insecticide container.
A quarter of a century before Mishra’s black day, Rajani Baraily, her younger brother and her parents survived similar poisons, but they now live with disability.
At the time, the Barailys lived in Kolkata’s Behala suburb, where they had bought rapeseed oil from a local ration shop. It contained triorthocresyl phosphate, a highly toxic additive. They used the oil for about a fortnight before starting to experience the contaminant’s toxic effects.
The Barailys suffered bouts of diarrhoea and strange sensations in their legs. “We felt very weak in the legs, as if our legs did not belong to us,” recalled Rajani. She was 13 at the time.
“A few weeks later we learned that it wasn’t just us,” said Rajani. “Hundreds of people in our area were suffering the same symptoms—marking the onset of paralysis. We were victims of rapeseed oil adulteration.”
The Behala tragedy left the Barailys permanently dependent on crutches. It has gone down in the annals of food safety, or notoriety, as one of India’s worst-ever cases of food adulteration.
Three days ago, at the other end of the country, 58 students of a government medical college in Thanjavur, Tamil Nadu, fell ill after eating breakfast at the canteen. “We cannot say anything for sure now,” said P G Sankaranarayanan, Dean In-Charge. Food samples have been sent for testing, and the poisoned students are stable.
The Thanjavur students were lucky because the adulteration of food—wilful or negligent—is one of those unchanging Indian tragedies, playing out with regularity, driven as it is by uncommon greed.
The uncommon greed of common people
Vijay Bahadur can tell you how an unwavering greed for profits takes hold of common people.
Bahadur is deputy commissioner with the Food Safety and Drug Administration, Government of Uttar Pradesh. On January 8, 2015, in Meerut, he confiscated more than 23,000 litres of non-edible oil from traders with licenses to produce mustard oil.
“Traders were passing off non-edible oil of different commodities, other than mustard, costing about Rs 25 a litre, for mustard oil, which costs up to four times as much, with a little help from artificial essence and butter yellow, a substance that makes oil look like mustard oil,” Bahadur told IndiaSpend.
Bahadur admitted to having been taken by surprise—not by the illicit activity but by the traders’ brazenness. “All traders care about is pocketing huge profits,” he said. “They show absolutely no concern for public health. On that day, they were openly selling the adulterated oil and aggressively opposed legal sampling for quality checks.”
The district administration had to provide Bahadur’s team with police guards.
Over two days, Bahadur and his team found more than 28 quintals of broken rice, more than 30 quintals of rice husk and synthetic colours.
Traders used these materials and colours to add volume to spices. “We even found a representative of Maharaja, a so-called reputed spice-brand based out of Kanpur, engaging in such malpractices,” he said.
The traders do not fear the law. Their focus is how to sidestep it and hoodwink authorities. One method is to sell contaminated oil under various brand names. If one is investigated, the others continue.
“It takes them no time at all to introduce a new ‘brand’,” said Bahadur.
The poisons in our food
Across India, this uncommon greed, it appears, is quite common. Research studies reveal a variety of contaminants in food substances across the country.
Milk is one of the most commonly adulterated food items. In a nationwide study of 1,791 milk samples conducted in 2011, 68.4% of the samples departed from Food Safety Standards Authority of India standards.
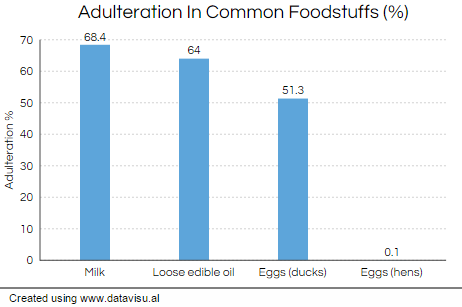
Source: FSSAI, Consumer Guidance Society of India, research
The study found detergent in 103 samples and skimmed milk powder in 548 samples. Water was identified as the most common adulterant. Cheating was just over twice (68%) as high in urban areas vis-à-vis rural areas (31%). All of the samples from Bihar, Chhattisgarh, Daman and Diu, Jharkhand, Orissa, West Bengal and Mizoram were substandard.
Citywide milk surveys put out different percentages of adulteration. A 2014 study of 50 milk samples supplied to cafes, small hotels and public and educational institutions in Hyderabad found sucrose and skim milk powder in 22% and 80% of the samples respectively. Urea, neutralisers and salt were present in 60%, 26% and 82% of the samples respectively. Formalin, detergents and hydrogen peroxide were present in 32%, 44% and 32% of samples.
Mustard oil (and other edible oils) blended with the oil of Argemone mexicana seed, a poisonous plant commonly called Mexican poppy, has been the subject of many a study. Mustard oil contaminated with Argemone oil is known to have caused dropsy—proteinuria or loss of albumin leading to edema of the extremities—on an epidemic scale in India as far back as 1877.
“Poisoning with Argemone oil can also cause headache, nausea, diarrhoea, erythema (a sensitive reaction of the skin), glaucoma (an eye disease) and breathlessness. In severe cases fatalities are reported due to congestive heart failure,” Dr Saurabh Arora, founder, foodsafetyhelpline.com, a research initiative founded by a food-testing laboratory, told IndiaSpend in an email interview.
Corrupt traders use Argemone seed oil to adulterate mustard oil because it is easily available, cheap and completely mixes with mustard oil. Not surprisingly numerous dropsy outbreaks have been reported in modern India.
One of the worst occurred in Delhi in 1999, when 3,000 people were hospitalised and 60 died. Most of the victims were very poor, people who bought the oil for cooking from local vendors. Another was reported from Dholkhakhara village in Panchmahal district of Gujarat in 2012.
Last year the Consumer Guidance Society of India declared that 64% of the loose edible oil sold in Mumbai is adulterated. The study tested 291 samples of sesame oil, coconut oil, groundnut oil, mustard oil, sunflower oil, cottonseed oil and soyabean oil.
A 2013 Baroda-based study of 40 food samples found higher than acceptable levels of arsenic in cereals, pulses, vegetables and roots and tubers. It also found higher than acceptable levels of cadmium in cereals, fruits and curd.
Arsenic poisoning can have a variety of adverse health effects, including death. Cadmium poisoning, similarily, has dangerous effects, including pulmonary disease and cancer.
Vegetable contamination as a result of contaminated irrigation water does not amount to wilful adulteration. But it is adulteration all the same.
Adulterated food includes substandard food because of inferior raw material or second-rate processing methods or inaccurate storage or packaging. Adulterated food also includes misbranded food and foods containing any sort of contaminant, whether added by design or by mistake.
In 2013, researchers investigating egg contamination in Bareilly, Dehradun and Izatnagar found traces of salmonella bacteria in 5% of the eggs sampled. A 2011 study in Kottayam found 1.33% salmonella contamination of the egg content for commercial layer hens, 2% for backyard raised layer hens and 51.33% for ducks. Ducks eggs are a local favourite.
And the most defining study of all: 13,571 of 72,200 (18%) samples failed food safety authority prescribed quality standards in laboratory tests conducted during 2012-13. Yet only 3,845 of 10,235 cases of adulteration were convicted.
What India needs: more convictions and deterrence
Stemming the poisons being thrust upon unsuspecting consumers in India is challenging. Since health is a state subject, the law has to be enforced by state food and drug administrations. It doesn’t help that most states lack sufficient food safety infrastructure.
In mid December, 2014, authorities announced the start of a six-month-long nationwide survey and testing of food samples in January 2015.
“But India doesn’t need more surveys,” Bejon Misra, an international consumer policy expert said. “India needs more convictions and deterrent penalties, imposed even before court proceedings get underway.”
Misra, the man behind the Jago Grahak Jago (wake-up consumer wake-up) campaign, was a member of the Food Safety & Standards Authority of India from 2006 to 2013. He represented the interest of consumers.
“It was an extremely disappointing experience,” he said of the stint.
“I can safely say the food authority has not taken any such steps in the interest of consumers,” said Misra. “It has become an authority to reward certain government officials. It has become a namesake authority (sic) accountable to none.”
Centre and state pass the buck, do not respect timelines on the implementation of food safety and standards law and compromise the “urgent need” to establish food-safety standards, he said.
To the question: do consumers stand a chance when traders with malicious intent abounds? Misra said: “In 1986, the central government had amended the Prevention of Food Adulteration Act and authorised every citizen to become a food inspector and participate in the task of food safety. But it failed to implement much-needed citizen capacity building measures. So consumers continued to be at the mercy of the food regulator. Recourse lies only in an honest endeavour by the regulators to empower our 1.3 billion consumers.”
Food safety, it appears, boils down to what you and I know, which is not a whole lot.
So, what’s safe to eat?
Awareness starts with knowing what to suspect.
According to the Food Safety & Standards Authority of India, daily use foodstuffs that are most prone to adulteration and contamination include milk products (khoya, butter, ghee, milk-based sweets), pulses like arhar and rajma, mustard oil, groundnut oil, poultry and meat, and fruits and vegetables.
Adulteration is rampant in products sold loose.
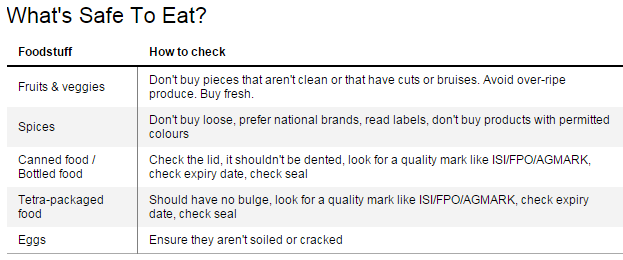
Packaged products from national brands are likely to be safer, since companies are more concerned about their reputation and brand loyalty. “Buy packed and labelled produce because it is more likely to be genuine and packaged in hygienic conditions,” said Bahadur. “Read the label declarations on the packet.”
Amarjeet Singh of the department of community medicine at Chandigarh’s Post Graduate Institute of Medical Education and Research has co-authored a study examining consumer awareness about food-purchasing practices.
“We found that more than 97% consumers are not performing essential checks,” said Singh. “Consumers must check fruits and vegetables for freshness, cleanliness, cuts, bruises and ripeness.”
His advice: Check the seal and expiry date of canned and bottle foodstuffs. Look for a quality mark—of FPO, ISI or AGMARK—and ensure the lid is dent-free and bulge-free. Make sure eggs are not soiled or cracked.
Common immediate symptoms of food adulteration are fever, vomiting, diarrhoea, pain in the abdomen, nervous debility, paralysis and if left untreated, death. Over a long period of time, foodstuffs laced with toxic substances can cause some cancers, hormonal imbalances, kidney damage, liver disease, or stunt growth.
Stay vigilant. Stay suspicous. A 2014 multi-city food safety survey conducted by Research Pacific for Tetra Pak showed that more than 70% mothers do not immediately connect serious diseases such as jaundice, cholera and typhoid with food safety.
Should you develop symptoms, don’t delay medical treatment. It could cause major complications.
Shalini Joshi, internal medicine consultant at Fortis Hospital, Bengaluru, told IndiaSpend of a man who fell sick after eating contaminated food on his travels but could not seek medical attention until he returned home.
“Severe diarrhoea had led to acute dehydration,” said Joshi. “He was admitted but soon shifted to the ICU because we found that his kidneys had been affected. He had to undergo dialysis a few times to help him recover, which he eventually did.”
Raw food—salads and fruit—are best avoided out of home. Well-cooked food is safer.
From tragedy, some responses
Scores of children—about 120 million across India—eating midday meals continue to be at the mercy of the respective state education departments. The only good to emerge from the Saran tragedy is some remedial action.
In an interview to IndiaSpend, Susanta Biswas, a senior consultant for the midday meal scheme of Tripura’s Education Department emphasised the need for quick action when the worst happens.
“Only five pupils took ill after eating the midday meal at Noapara, but we still rushed all the children, 42 in all, to the hospital,” said Biswas. “We kept the sick students overnight and discharged them the next day after they had fully recovered. All the rest were discharged immediately after a check-up. You can’t take chances.”
A probe revealed a dirty kitchen and kitchen ingredients purchased individually. Noapara’s kitchen has since spruced up. State authorities also started to more closely inspect kitchens in other schools.
“This fiscal, we have punished 280 school heads for negligence,” said Biswas.
Some interest is better than no interest.
Back in Kolkata, Rajani, her family and hundreds of others continue to battle their disabilities.
After being struck down with partial paralysis, the Baraily family spent an agonising year in two hospitals. That helped them to regain some strength and mobility in their arms. Rajani went back to her studies.
Lately, she's tried to find a job but failed. The state government gives the family Rs 300 each as compensation each month.
“I feel numb, not angry," said Rajani. "What bothers me is why doctors don’t have a cure for us."
In Bihar, Akhilanand Mishra is an angry man, waiting for justice.
“I want nothing less than the death sentence for the guilty,” said Misra. “They promised us a fast- track trial. Eighteen months have passed and there’s been no conviction.”
Update: The data on the number of samples failing food-safety authority tests have been revised.
__________________________________________________________
“Liked this story? Indiaspend.org is a non-profit, and we depend on readers like you to drive our public-interest journalism efforts. Donate Rs 500; Rs 1,000, Rs 2,000.”


