In J&K Shutdown, PM’s Health Scheme Grinds To Halt, Healthcare Crisis Grows

Srinagar: His eyes puffy, his spirits low as he lay on a hospital bed with tubes running out of his body to a dialysis machine that purified his poisoned blood and sent it back, shawl vendor Niyaz Wani contemplated how much longer he could afford his treatment.
Till August 26, 2019, Wani’s dialysis was free of cost at the 50-bed Khyber Hospital, one of Srinagar’s leading private medical institutes. He is a “golden card” holder under the prime minister’s key medical-costs reimbursement programme, the Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (national health protection scheme), which--until August 2019--reported the best use nationally in Jammu and Kashmir.
Started in September 2018, Ayushman Bharat provides free health services costing up to Rs 5 lakh (Rs 500,000) to over 100 million Indian families who live below the official poverty line. Wani was one of those--until last week, when the hospital suspended free treatment because it could not register and process claims on the internet, which has been blocked by the government for 31 days now.
Wani was not alone in the 20-bed dialysis centre. Almost all the other patients we met were golden card holders: rickshaw drivers, labourers and other daily wage earners struggling to get dialysis now that Ayushman Bharat services were down. Even though they needed dialysis, some patients were going to discontinue the treatment because they could not afford it.
On humanitarian grounds, the Khyber Hospital allowed free services for golden card holders until August 26, 2019, believing the internet would be restored. But with current unpaid bills running to Rs 22 lakh and Rs 60 lakh yet to be received from the central government, hospital authorities said they had now stopped free treatment for Ayushman Bharat beneficiaries.

Patients in the dialysis unit of Srinagar’s Khyber Hospital. Most patients are beneficiaries of the Pradhan Mantri Jan Arogya Yojana, the prime minister’s national health protection scheme, and received free treatment. Since August 26, 2019, when the hospital stopped free medical care because of mounting bills, patients have had to pay. Some are ceasing treatment.
Wani said he had to now pay Rs 2,500 per dialysis or about Rs 20,000 per month, excluding medicines. “I had to sell my wife’s gold ear-rings to afford treatment,” he told IndiaSpend from his hospital bed. “I got just Rs 15,000 for that pair of ear-rings. It was more than 1 tola (10 gm of gold). These goldsmiths are very smart, they are not giving loans but asking us to sell [our gold] instead.”
Since August 5, 2019, when India’s parliament passed legislation to abrogate Article 370 of the Indian Constitution--introduced in 1949 as a condition for Jammu and Kashmir to join India--deployed an additional 38,000 troops and suspended telephone and internet services in the Kashmir valley, a healthcare crisis is increasingly evident.
Ayushman Bharat patients cannot access free services. The private and government hospitals we visited were half empty. MRI machines could not get software updates. Many drugs were in short supply, and with courier services suspended, those who could afford to were making journeys to Jammu, Chandigarh or Delhi to fetch medicines. Surgeries were postponed or curtailed. Doctors were idle. Patients in need of life-saving procedures may have died--but there is no way of knowing because of the continuing mobile and internet blackout.
On September 4, 2019, a month since the communications blockade, Srinagar’s district magistrate and development commissioner Shahid Choudhary retweeted the official Twitter handle of the state’s information and public relations department that said: “100% of landline exchanges to be operationalized; Remaining 19 exchanges being opened tonight”. Mobiles are being “restored gradually” and “already buzzing in Kupwara”, Choudhary added. He also said surgical procedures in hospital were normal and medicines available.
Much of this had not happened when this story was written on September 5, 2019.
At the Khyber Hospital, Wani told us how he earned Rs 500 per day during tourist season and how he had no income since August 2019 when shops and businesses in the Valley were shut down, an unofficial civil strike to protest against the government’s decision to abrogate Article 370 and downgrade Jammu and Kashmir from a state to a union territory.

Businesses and commercial enterprises have been shut in Kashmir since August 5, 2019, as part of a civil strike to protest the Centre’s decision to abrogate Article 370 of the Indian Constitution and downgrade Jammu and Kashmir from a state to a union territory.
“My three children will have to stop their studies,” said Wani. “There is no money even to buy rice or vegetables now.”
“Why are poor Kashmiris not able to avail benefits of Ayushman Bharat when all other Indians can?” asked Wani.
‘We don’t know how many died’
Before August 5, 2019, the Khyber Hospital averaged 30-40 angioplasties--procedures to treat blocked blood vessels in the heart. Last month only about 10 angioplasties were conducted, said a senior cardiologist, not willing to be identified for fear of being persecuted. Most officials in government hospitals, hospital owners and doctors told IndiaSpend that they had been instructed by the government not to speak to the media.
“See, heart attacks still happen, they don’t stop. In fact there could be more because of the [additional] stress,” said the senior cardiologist. “What has happened now is that patients are not able to reach to the hospital. This particularly happened in the first three weeks following the clampdown. Many may have died, but there is no way to know.”
Even at the Shri Maharaja Hari Singh (SMHS) Hospital, one of Srinagar’s top two government hospitals, doctors said neither could patients with scheduled surgeries reach the hospital nor could the hospital administration contact them.
Many hospital employees living away from the premises could not make it to work because of security barriers. Many surgeons we spoke to decided to not operate on “high-risk cases” because there was no way for the resident doctors to contact senior consultants in case of emergency.
Hospitals have started using ambulances to ferry hospital staff to and from work because in some areas private vehicles are not allowed to proceed. Routes are pre-set, but during emergencies, without mobile phones, it is difficult to reach doctors.

Ambulances are used to ferry doctors and hospital staff to and from hospitals in Kashmir due to security concerns and a lack of public transport.
The government has claimed that landlines have been restored in some parts of the Valley, especially in government offices and police stations.
However, there was no working landline at SMHS Hospital when IndiaSpend visited on September 4, 2019, even though it had been officially restored on September 1, 2019. Hospital staff said the mobile phone of the head of the hospital, Parvaiz Ahmad Shah, who also heads four other hospitals in Srinagar, was working.
IndiaSpend tried to meet Shah three times at his office, but he refused to meet us or offer comment.
At the directorate of health services, many landlines were not working on September 4, 2019. Only the mobile phones of the health director and district chief medical officers had been restored. Other emergency staff in Srinagar and other district hospitals did not have access to mobile phones or landlines, IndiaSpend has learnt.
Patients hitch rides, borrow vehicles
Most patients in rural Kashmir depend on tertiary hospitals in Srinagar for their health needs. With communication services down, heightened security checks and no public transport, patients from rural areas cannot easily reach the city. We met patients who hitched rides, borrowed vehicles from neighbours and relatives, and spent a lot of money to reach the hospitals.
Altaf Ahmad Sheikh, 45, who had piles, was taken to SMHS hospital by his son on a motorcycle from Tahab-Pulwama, 60 km south of Srinagar. “We could have come in a bus if the situation was normal,” Ahmad said, adding that doctors told him to revisit the hospital in October for a surgery.

Shri Maharaja Hari Singh Hospital in Srinagar. Outpatient numbers at one of the city’s leading government hospitals have fallen by about half since August 5, 2019.
Another patient, Abdul Subhan Lone, said he paid a neighbour Rs 200 for fuel to get a drop to the highway from his village of Payipora in Tangamarg. “From there, I hitched a ride in three vehicles to get here,” Lone said.
Doctors at hospitals in Srinagar told IndiaSpend they were deferring surgeries, except emergencies and deliveries.
Out-patient department data indicate how services have been affected.
Here are some post Aug 5 details of surgeries:
— Shahid Choudhary (@listenshahid) 29 August 2019
LD hospital -1168, SMHS -682,
Bone and joint hospital -800,
Superspeciality -382, SKIMS -410. Total -3442
It's absolutely in consonance with our monthly average this year.
When IndiaSpend visited Sheikh Ul Alam Hospital, a private hospital in Srinagar, it was deserted. The out-patient department (OPD) was empty and a display board said that only three patients were admitted in the 20- bed facility. The hospital usually receives 350 patients every day in its OPD but has received only 50 each day since August 5. Instead of 300 surgeries every month, it had done only 50 in August.

The lobby of the Sheikh Ul Alam hospital in Srinagar. The hospital conducts 300 surgeries, on average, every month. In August 2019, it conducted less than 40. When we visited, there were only three patients admitted in the 20-bed hospital.
This is because even if patients come to the hospital, its doctors now refer patients to a government hospital, which have an anaesthetist and surgeon present at all times. Finding doctors during emergencies without a phone is a risk the hospital is not willing to take.
The internet shutdown affects medical equipment.
At the Shafie Diagnostic Centre, a public-private partnership at the Bone and Joint Hospital, the MRI machine--one of three in government hospitals here--suffers glitches, but it is not getting its software updates and company technicians have not been able to find out what is wrong.
In normal circumstances when a problem is evident, the diagnostic centre sends photos of the MRI machine’s screen to the company through WhatsApp. The problem is usually “promptly resolved”, staff at the diagnostic centre said.
Drug shortages, refrigeration problems
Ishitaq Lone, 54, was perspiring when we met him at a chemist shop in the city. Asked if he could find medicines, he grew angry.
“I have been searching for these medicines for the last one week, I have visited at least 20-25 shops,” he shouted. The drugs he was looking for are commonly prescribed for diabetes--Glized, Innomet and Janumet.
Lastly, I see people getting angry and abusive finding rebuttal of such panicky reportage. Instead of that bring cases to my knowledge, I assure personal attention even as 94% doctors are on duty.
— Shahid Choudhary (@listenshahid) 29 August 2019
Lone, his mother and his father are diabetics. His medicine stock, bought on August 4, 2019, had run out. Without his oral diabetes medicines, he was taking increased insulin doses to manage his disease.
“Already, our blood glucose tests have shown higher than usual levels, I do not want to check it again because it will stress me out,” said Lone, who was planning to go to Jammu to buy these medicines.
The drugs Lone required are currently unavailable, confirmed Farooq Ahmad, a chemist. “Since the last 10 days, there has been a shortage of diabetes drugs and insulin,” he said.
All concerns and worries are deeply appreciated but we were not low on medical stocks even for a single day. No interruption in supplies. Still open to help individual cases, if any.
— Shahid Choudhary (@listenshahid) 23 August 2019
https://t.co/MZDlX8bDNC
Distributors cannot reach their main drug suppliers and are finding it difficult to convince truck drivers to bring the drugs to Kashmir because of security concerns. “I finally brought the drugs in my own car from Chandigarh, but I had to pay a Rs 5,500 challan (fine) because it is not allowed,” said Ishwaq Ahmad, a distributor.
Medicines in particularly short supply are ones that need to be refrigerated and delivered within 24 hours, such as vaccines, insulin and some cancer formulations. “This is because courier companies have refused to operate in Kashmir,” said Mushtaq Ahmed Pukhta, distributor and office bearer for the Jammu & Kashmir Chemists and Distributors Association. If the current situation persists, there will be a definite shortage of these drugs, he added.
Distributors had complained to Kashmir’s drug controller 10 days ago, said Pukhta, but nothing had been done yet.

Vaccines, cancer drugs and insulin are in short supply in Kashmir. If the current situation persists, there will be a definite shortage of these drugs, says Mushtaq Ahmed Pukhta, distributor and office bearer for the Jammu & Kashmir Chemists and Distributors Association.
Cancer patients look for medicines
There had been no change in the number of chemotherapy patients receiving treatment at a Srinagar private hospital, whose officials requested that it not be named. “That’s because our patients cannot afford to delay treatment,” said Uroosa Fayaz, junior resident doctor. “If they even miss one cycle, they have to repeat the whole thing again.”
The communication blockade has added to their difficulties.
Chemotherapy drugs, ordered when a patient needs them, are not easy to find. In one case, the hospital intervened, calling the medical supplier.
Fayaz spoke about a cancer patient who needed an immunotherapy drug, which a relative had to get from Delhi. It took one week.
“It was very challenging to organise the drug especially because there are no phones or internet working,” Fayaz said, noting that even a “few days’ delay” can be too much.
An oncologist at a government hospital, speaking on condition of anonymity, said she sent biopsy samples to pathology labs in Delhi but their results never came after August 5, 2019. She performed biopsies again for patients who returned, in local path labs, but many patients did not return. Patients who were not diagnosed and did not begin treatment will now possibly return in two or three months, during which time the cancer may have progressed.
The oncology department in the government hospital, which normally sees 200 patients a month, only got 50 patients in August 2019.
Full stop to Ayushman Bharat
There were 613,697 families--29% of all families in the erstwhile Jammu & Kashmir--eligible for Ayushman Bharat. Till May 2019, 1.1 million e-cards had been generated and 13,000 claims worth Rs 8.7 crore submitted, according to the Ayushman Bharat website.
The state had one of the best rates of utilisation of the scheme.
Hospitals treated patients cashless and free of cost by verifying card-holder details from the Ayushman Bharat website and waiting for “pre-authorisation”, after which the hospital got paid depending on the disease package chosen. This is required to be done within seven days.
Without the internet, hospitals have not been able to log on to the Ayushman Bharat website, so they have been turning away patients.
On August 28, 2019, the nodal agency for the scheme in Kashmir issued a circular that under the “exceptional circumstances”, the documents could be uploaded even after the seven-day period.
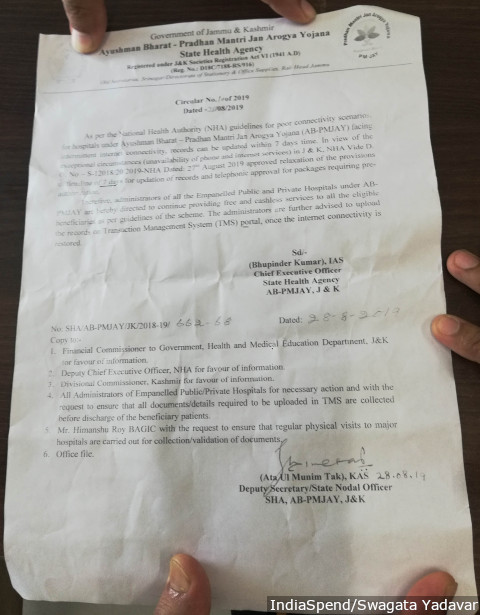
A government note on August 28, 2019, mentions “exceptional circumstances” in relaxing a seven-day deadline to update patient details on the website of the prime minister’s health insurance scheme. Patients in Kashmir have not got free treatment since August 5, 2019, when the government shut down the internet.
However, hospital officials we spoke to said this circular does not address the problems of verification, and hence they have still not resumed processing Ayushman Bharat claims.
“From August 28, we have started scanning the documents of the patients and making manual registration but they do not get free treatment,” said an employee at a government hospital, who had added only five patients since August 28, 2019. “Maybe they will get reimbursed when Internet connectivity resumes.”
"I haven’t seen or spoken to my children”
There was a rush of patients and attendants inside and outside the 200-bed Lal Ded Maternity hospital. At the entrance was a desk that said “announcer”. This was an ingenious idea devised by the hospital to get in touch with doctors and attendants who are impossible to reach in the crowded hospital without a mobile phone. Announcements told attendants if their patient needed them or if doctors needed to rush to see a patient.
In the second-floor lobby, Sara Begum, dressed in a light-green salwar kameez with hair covered by a dupatta, was chatting with another patient’s attendant. Sara Begum said she was here with her sister-in-law, who had had a caesarean-section, but she did not know when she would be discharged. They were from Tikipura Lolab, 110 km from Srinagar.
They had gone to their nearest community health centre, from where they had got an ambulance that dropped them at Lal Ded. She thought they would return in three days, but it had been six days. Sara Begum was anxious. “I haven’t seen or spoken to my children,” she said. “I can’t express how sad I feel.” There has been no way to communicate with her three children or husband, or to tell other relatives to come and relieve her.

Abdul Qayoom and his wife Shaista sit with a relative in the waiting room of Lal Ded Maternity Hospital, Srinagar. The family lives in Nowgam, 8 km from the hospital, but because of security barriers and dead phones, they prefer to stay in the hospital for two days after discharge than come back for follow-up. “This 8 km feels like 80 km to us,” says Qayoom.
A doctor’s walk to find his patient
On September 2, 2019, 27 days after the communication blockade, Omar Salim Akhtar, 38, a urologist at the Government Medical College, Srinagar, was worried about a patient he had not seen for a month. Gulam Mohammed, 85, had multiple ailments--hypertension, diabetes, some degree of renal failure and prostate enlargement.
Until a month ago, Mohammed often consulted Akhtar, coming to the hospital with one of his family members. Unable to call Mohammed or his family, Akhtar wanted to know if the patient was well.
After finishing 12 surgeries, Akhtar still had an hour of duty left. He decided to take a walk downtown, past the security barriers, and try to find Mohammed’s home. He walked 2 km to reach Fateh Kadal, a neighbourhood under a stifling lockdown.
Akhtar remembered Mohammed telling him he lived across the bridge. “I crossed the bridge, took a left and walked to the next lane,” said Akhtar, a lean man in a polo shirt, sporting a stubble. “Thankfully I saw Mohammed’s grandson on his cycle. He said, ‘What are you doing here, Doctor?’ I told him I had come to see his grandfather.”
Once inside, Akhtar found that Gulam Mohammed was doing alright. He walked back to his hospital.
In a city dotted with security bunkers and thousands of security personnel after the security clampdown since August 5, 2019, walking to Srinagar’s downtown was fraught with risk, but that did not deter Akhtar.
Akhtar is the doctor whose video went viral, after he was arrested--he was released two hours later--in Srinagar’s press enclave on August 26, 2019, after he told the media how the communications blockade was affecting his patients.
“This is not a protest, this is a request,” he had written on a placard. He said he had wanted to bring to attention the hospital’s inability to process Ayushman Bharat claims because there was no internet.
“Due to the lack of internet and phone connectivity, we are unable to provide [free] treatment since the past three weeks,” Akhtar had said previously. “Therefore, I have seen my own patients and other patients spend from their pocket to pay for their dialysis, chemotherapy, etc.”
Akhtar’s efforts resulted in the August 28, 2019, circular that allowed a relaxation of the seven-day deadline.
Doctors are idle, as a need for them grows
An unusual sight caused by the communication clampdown is doctors and surgeons idle for hours. We found paediatricians, cardiologists, orthopaedics and general physicians chatting over cups of tea in private and government hospitals.
With very few surgeries and fewer outpatients, doctors have time on their hands, at a time when patients need them.
“Government hospitals in Srinagar have enough (medicine) stocks to last for eight months,” said the head of urology at one of Srinagar’s government hospitals. “What is missing are the patients.”
He sat in the hospital canteen with the head of paediatrics. There were six tables with cheap plastic covers, and the doctors had just finished their lunch.
“There is no way to know what happened to patients who were supposed to come for a follow-up but did not turn up,” the urologist said.
Two younger consultants joined in, and the doctors discussed how to deal with the dichotomy: idle doctors in hospitals and patients at home waiting to get to the hospital.
“I have proposed this to a private hospital--if they get patients who require surgeries, I will do the surgery for free,” said the head of paediatrics. “If a surgery costs Rs 40,000, we can slash our fees and only charge for the equipment and medicines, the cost can come down to around Rs 6,000.”
The head of paediatrics then showed some papers—he was planning voluntary retirement and a move to the United Kingdom. He had trained there but chose to return to Kashmir, refusing an offer in the United Arab Emirates. After August 5, he said he wanted to leave.
This is the first of a three-part series. You can read the second part here and the third part here.
(Yadavar is a special correspondent with IndiaSpend. Parvaiz is an independent journalist based in Srinagar.)
We welcome feedback. Please write to respond@indiaspend.org. We reserve the right to edit responses for language and grammar.


