Why COVID-19 Surged By 59% In Two Weeks Among Assam’s Health Workers
Guwahati: Negligence in testing out-patients in hospitals, staff shortages leading to prolonged exposure to the sick, and indiscriminate admission of all cases--asymptomatic, mild or severe--to health facilities. These are the factors that caused a spike in the number of COVID-19 cases among Assam's health workers starting from May. The spike intensified in August, increasing from 720 on July 28 to 1,143 by the second week of August--a 59% rise--health workers told IndiaSpend.
The first COVID-19 case in Assam was reported on March 31 and by July 27, 720 health workers had tested positive in the state, S Lakshmanan, the state director of the National Health Mission (NHM), Assam had told IndiaSpend on July 27. On August 10, NHM officials at a plasma donation drive reported that 1,143 health workers had contracted COVID-19--a rise of 59% in about two weeks. Of those affected, two cases turned fatal--both doctors.
At the obstetrics/gynaecology department of the Guwahati Medical College and Hospital (GMCH), the biggest government hospital in the Northeast, doctors have been so overworked that three doctors are handling the work of 10, said an obstetrician-gynaecologist who chose to remain anonymous. On July 19, Abhijit Sarma, the GMCH superintendent and associate professor in the department of surgery, tested positive for the virus but has since recovered.
Of the 1,143 health workers who contracted the virus, 298 were doctors, as per Lakshmanan, making this the worst-affected single category. This was followed by nurses (162), cleaners (125) and lab technicians (92). The highest (311) numbers were reported by those clubbed together as “other health workers”--ambulance drivers, data entry operators, emergency medical technicians, district administration and ASHA workers.
In July, the Assam chapter of the Indian Medical Association (IMA) demanded an inquiry into why “so many health workers and doctors were affected by the disease while working with the disease”.
At Guwahati’s short-staffed COVID-19 facilities, the health workers we spoke to reported being overworked and anxious about contracting the infection, as we detail later. They also complained about substandard infrastructural facilities and chaotic administrative decisions that added to the crisis.
Until July, out-patients were not being tested before consultation at the GMCH, said the obstetrician-gynecologist who spoke to IndiaSpend. This was despite the community spread in the city and GMCH’s categorisation as a dedicated COVID-19 hospital. “Now we’re testing patients but if someone comes in active labour, we can’t wait for the test results from RT-PCR,” said the doctor. “We have done about 20 deliveries without knowing the status of the patient or have just operated after a negative rapid test result.”
Of the 298 doctors affected, 128 (43%) are from Kamrup Metro, as per Lakshmanan. A total of 166 health workers have tested positive in the district, of which 66 are from the government sector, as per Ganesh Saikia, joint director of the health department in Kamrup Metro.
Kamrup Metro is the biggest commercial district in the Northeast, that includes Guwahati and state capital Dispur, and a medical hub for the region. The district has witnessed a spike since May when migrants outside the Northeast started returning and the lockdown was first eased, with numbers going up from four on May 8 to 16,105 by August 5.
However, Samiran Das, registrar at the department of endocrinology who served in the superspecialty COVID-19 ward at GMCH, maintained that only four doctors had contracted the virus while on COVID duty. “The rest were infected from general wards in the hospitals. This is why we made antigen tests mandatory for all our patients and their attendants since the first week of August,” he said.
At the national level there are no official data on the number and category of healthcare workers who have tested positive. The last set of official figures--1,073 until May 23--were first released in the Indian Journal of Medical Research in June. In the same month, News18 collated data to find over 1,200 healthcare workers in Delhi’s major hospitals had tested positive since March.
In a review meeting on August 7, Lav Agarwal, joint secretary in the Union health ministry, reportedly told the Maharashtra government that the rate of infection among Maharashtra’s health workers--21%--was much higher than the national average of 7%. However, the source for Agarwal’s estimates was not traceable.
By August-end, Guwahati will have an estimated 30,000 cases and the entire state 65,000, state health minister Himanta Biswa Sarma said mid-July. However, with a reported doubling time of 15.9 days on August 8, when cases in the state climbed up to 57,714, the COVID-19 count could cross 110,000 by August 24.
Taking note of the impending crisis, on August 9, Sarma announced free medicines and pulse oximeters for patients opting for home isolation. This indicated a change in the state policy to not encourage home isolation--in a July 1 notification, it was stated that a patient opting for home isolation had to agree to arrange for a caregiver, a pulse oximeter and a private vehicle to deal with emergencies. The patient was also required to give an undertaking that the government would not be responsible for any health consequences.
Despite a strict three-week lockdown in Kamrup Metro district, the number of daily reported cases did not see any significant decline.
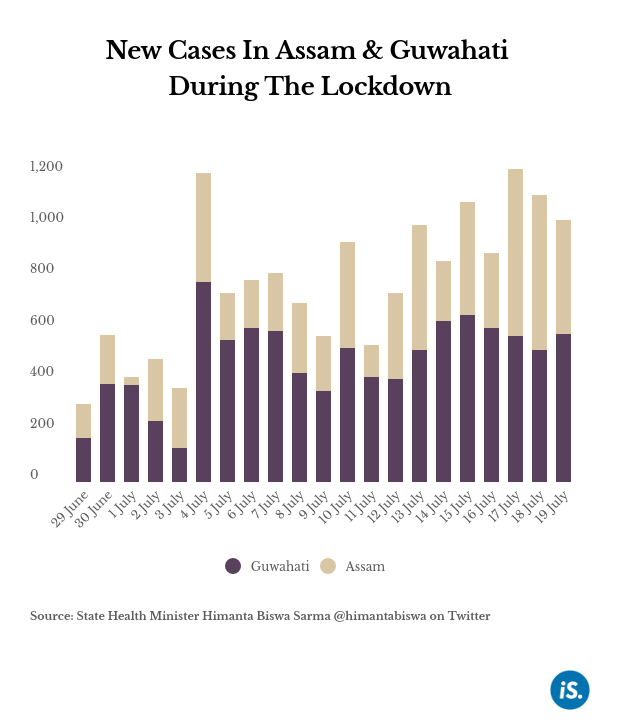
Since July 20, offices and businesses have resumed at 30-50% capacity in the first phase of the easing of the lockdown. As of August 5, Assam had 15,900 active cases, and 121 deaths have been reported since the pandemic first hit the state in April. Of these, 4,720 active cases and 46 deaths were reported from Kamrup Metro.
The state recorded its highest single-day spike of 4,593 cases on August 12, when the maximum number of tests--143,109--were conducted, of which 632 (highest in the state) new cases were detected in Kamrup Metro. The recovery rate (65.3%) is below the national average (70.77%). The state’s fatality rate of 0.23%, however, is about a tenth the national average (1.96%). The corrected case fatality rate, or the number of deaths among 100 COVID-19 cases with known outcomes, is still among the lowest in the country--0.36%, compared to the national average of 2.7%.
Indiscriminate admission of all COVID-19 patients
On July 7, the state chapter of the IMA advised the government to adhere to guidelines prescribed by the Indian Council of Medical Research on the management of COVID patients, which recommended institutional care for only those “clinically assigned” as very mild/mild, moderate or severe.
The July government notification clarified that it was discouraging home quarantining because it does not have enough personnel to monitor those in home care and not enough ambulances to rush them to health facilities if they turned critical. “We’ve [also] seen so many cases where even if a patient isolates himself, his family members are roaming about the city,” said Samiran Das of GMCH, explaining the government decision.
But other doctors that IndiaSpend spoke to said that the state’s healthcare system was overburdened by the admission of asymptomatic and mildly symptomatic individuals to COVID care centres and hospitals.
At the current rate of infection spread, the COVID care beds would soon run out, said a resident doctor at the Patanjali Yogpeeth Mirza, classified as a COVID-19 care centre in rural Kamrup but also takes on cases from Guwahati. “There’s not much social distancing being practiced in COVID care centres,” said the doctor who did not wish to be named.
The government has finally responded to doctors’ demand only when they saw no decline in the number of those infected, said Hemanga Baishya, state secretary of the Assam chapter of IMA. “They cannot expand the number of beds in COVID care hospitals on a daily basis. Even the increase in beds would require manpower to run it,” he told IndiaSpend.
Rest and test rules
On July 6, the state’s health and family welfare department had asked medical teams on COVID duty to undergo rapid antigen testing after 11 consecutive days of work, followed by three days of home quarantine if the result is negative. The IMA protested against the decision, which they said would “demoralise frontline workers”.
Antigen tests have low sensitivity and the results have to be confirmed by an RT-PCR, the association said. The department then revised the notification to a roster of seven days of duty followed by seven days of quarantine upon a negative RT-PCR test result.
Even though the IMA did not discriminate between the different kinds or grades of healthcare workers in terms of quarantine conditions, the revised guidelines only applied to doctors in critical care units, Das said, adding that they were meant for those attending to “serious patients” but not for those dealing with mild/asymptomatic patients in COVID care centres.
Lab staff overworked
In May, IndiaSpend reported on Assam’s low rate of testing (425 samples per million population) despite the highest number of testing centres and capacity in the Northeast. In June the Assam government stepped up testing significantly--as of August 13, 1,573,800 samples (45,893 per million population) were tested in Assam, as per the state COVID bulletin. The state has a positivity rate of 4.4%, lower than the national average at 8.93%.
The state has conducted 686,305 antigen tests, of which 123,201 were done in Kamrup Metro. Of these, 7.08% were positive, higher than the 5.19% in the state. Apart from the reverse transcription-polymerase chain reaction (RT-PCR) and TrueNat tests, the Indian Council of Medical Research approved, the antigen-based Standard Q COVID-19 Ag significantly helped raise the testing rate in Assam.
However, this accelerated rate of testing has increased the work pressure for technicians in laboratories, said Navanil Barua, the director of neurosurgery, GNRC (formerly known as Guwahati Neurological Research Centre), a private hospital in Dispur. “The government says Assam ranks very high in testing but there’s a price to pay for that. So many in the microbiology department of GMCH are getting sick because they are overburdened with work,” he told IndiaSpend.
Atanu Boro, 36, a lab technician with the GMCH, had been working nine-hour shifts since May 2020, collecting and testing hundreds of samples daily for COVID-19. On July 18, he tested positive for the disease.
“Soon after I started doing the rounds with the mobile team testing health workers on COVID duty, I began feeling weak though I didn’t have a fever or cold,” he told IndiaSpend. Boro remained asymptomatic but he was anxious for his pregnant wife, who is a health worker too. He had to return to work after serving a one-week home quarantine after hospital discharge, as required by Assam government rules.
Lab technicians like Boro, dressed in cumbersome personal protective equipment, work nine hours a day for 10 consecutive days collecting and testing 100-150 samples a day. At the end of 10 days, they are tested by RT-PCR and upon a negative result, asked to do a seven-day home quarantine.
“Until there’s a vaccine, we don’t have any option [but deal with long work hours] and also we’re short on staff,” he told IndiaSpend.
Trained technicians the government hospitals had “borrowed” from the private sector have gone back to their private labs to test samples, said Barua of GNRC.
With the goal of testing 5,000 samples on a single day in the city, the government has prioritised the recruitment of lab technicians. “Our administration has, also, been helping us with manpower, especially lab technicians, from other districts,” said Preety Rekha Dutt, district programme manager at the state NHM. Three weeks ago, the state NHM announced 150 vacancies for lab technicians. Lakshmanan confirmed that all the vacancies had been filled out and “more lab technicians were recruited in the previous months”.
Not enough hands for contact tracing
Not only is there a shortage of staff in pathological laboratories and patient care, but also of health workers needed for contact tracing and testing. This includes lab technicians from GMCH and NHM officials along with community workers or ASHAs.
In a survey released in June by Article-14 and Behanbox, ASHA workers across the country, including Assam, complained about not being paid their monthly honorariums or the centrally announced COVID incentive of Rs 1,000, on time. Even as India passed the 2-million cases mark on August 6, over 3 million community workers staged a country-wide protest demanding better incomes and timely payment of government incentives and insurance where deaths have occured.
NHM’s Preety Rekha Dutta said that with the high number of cases in Kamrup Metro, the district has run out of resources to trace and test all the contacts of every patient. Initially, in July, the Assam government deployed undergraduate medical students on COVID-19 duty, for contact tracing, and later shifted them to work at care centres.
Government officials that IndiaSpend spoke to admit that tracing has now been limited to mostly primary contacts. Biswajit Pegu, the deputy commissioner of Kamrup Metro, said that extensive tracing was possible when the cases were in single digits.
“Now we have opened up several screening centres and 12 hospitals where swab collections are taken. So the contact tracing is now restricted to the immediate neighbourhood of the positive cases,” he told IndiaSpend.
Stress, anxiety
In July, the World Health Organization said that health workers accounted for 10% of all COVID-19 cases globally, adding that “many health workers are also suffering physical and psychological exhaustion after months of working in extremely stressful environments”.
The rising number of cases among health workers is leading to cases of “stress, anxiety and panic” among health workers, said Sangeeta Dutta, a Guwahati-based psychiatrist. “Many are also under pressure from their families that are worried that they might bring the virus home,” Dutta told IndiaSpend. Given the mutating nature of the virus, health workers expressed fears about the “unknown”, she said.
Apart from counselling, Dutta has been prescribing anxiolytics (anti-anxiety) and antidepressants to healthcare workers who complain of panic attacks and insomnia. “Healthcare professionals are tired and burnt out now,” Dutta said. “Not seeing the results of their hard work for the last four months has especially affected their morale.”
With fresh recruitments, Boro has been spared the mobile unit duty he was earlier assigned for a few weeks. But he will be back at his task in less than a week. Despondency over the unknown timeline of the fight against the virus grips him at times, he said. “We’re working so hard, but we are yet to see any results,” he said.
(Sitlhou is a journalist based in Guwahati, Assam. She covers the Northeast region for several national and international publications. You can reach her on Twitter @makesyoucakes)
This story was edited by Malini Nair.
We welcome feedback. Please write to respond@indiaspend.org. We reserve the right to edit responses for language and grammar.